|
Al-Shifa Journal of???????????
|
||
|
Aims and Scope
Ocular Infections and Seasonal Variations Sensitivity of Tests in Dry Eyes Intravitreal Kenacort in Macular Edema ERG in Diagnosis of Retinal Problems |
Ophthalmoplegic Migraine; A case report and review of literature Tayyab Afghani, MBBS, MCPS, MS (Pak), DCEH(London), FIACLE(Australia) ? Purpose: To highlight the presentation and management of a case of ophthalmoplegic migraine and mini review of the subject. Study Design: Case report. Participant: A 12 years old boy presenting with painful unilateral, recurrent ptosis. Discussion: The incidence of childhood migraine in general has been estimated at between 2% and 5.7%.? The ophthalmoplegic migraine is quite rare and constitutes 0.16% of childhood migraine. Third nerve involvement is most common. A typical clinical syndrome emerges in a child or young adult with periodic headache associated with ophthalmoplegia involving all functions of the third nerve, beginning at the height of an attack of cephalgia, which is primarily unilateral and in the orbital region; the paresis lasts for days to weeks following the cessation of headache; recovery is gradual and tends to be less complete after repeated attacks. MRI may show enhancement of third nerve. Systemic steroids have shown promising results. The present case report is quite typical of those reported elsewhere: Al-Shifa Journal of Ophthalmology 2005; 1: 10-16 © Al-Shifa Trust Eye Hospital, Rawalpindi, Pakistan.
|
|
|
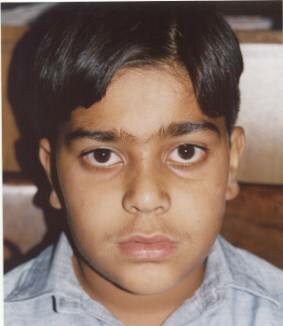
Case Report: 12 years old boy presented with 4-months history of severe episodic ipsilateral left sided headache along with pain in and around the eye, usually starting in the evening and lasting for 1-2 hours, improving mostly with vomiting followed by sleep. Five months after the start of these episodes, he started having mild swelling and moderate drooping of upper lid on the same side. This was associated with limited ocular movement especially in elevation and abduction. Interestingly the pain in and around the eye and vomiting was less marked when ocular motility disturbances started.? The child was brought to oculoplastic clinic when child began to have ptosis.? Clinically the eye examination was normal except for left upper lid ptosis, and limited abduction and elevation. The systemic examination was also normal. Radiological studies and serological examination was within normal limits. The child was diagnosed as a case of ophthalmoplegic migraine and put on 30 mg of steroids tapered over a period of three weeks. The child responded well and all symptoms and signs disappeared. Two weeks after the steroids were stopped, there was recurrence of the same. The child was again given the same dose and course of treatment.? The child is alright and symptom free for the last one year. Originally received: October 2, 2004 ? |
||
?????  ????????????????????????????????????????????????????????????? ?????????????????????????????????????????????????????????????  Left ptosis at presentation????????????????????????????? ?????????????????????????????????????? Limited elevation on left side ????? |
||
|
Discussion:???????????????????????????????????????????????????????????????????????????????????????????????? ????????????????????????????????????? The incidence of childhood migraine in general has been estimated at between 2% and 5.7%.1,2. Ophthalmoplegic migraine is a rare condition usually beginning in infancy or childhood and characterized by paralysis of ocular cranial nerves in association with vascular headache. The diagnosis is one of exclusion. Most patients should have high resolution magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA) to eliminate the possibility of aneurysm, tumor, or granulomatous inflammation Most of the cases of acute third nerve palsy and headache formerly referred to as "ophthalmoplegic migraine" show MRI enhancement of the nerve3,4.? It appears now that this entity is most like Bell's palsy in that it is an isolated "idiopathic" probably post-viral inflammation of a cranial nerve, the III.? The headaches may also be associated with other ocular motor nerve palsies as well5,6. Usually the ophthalmoplegia is transient; however, it can become permanent especially after repeated attacks. In this case, isolated, recurrent unilateral eyelid ptosis with some degree of reduced ocular motility was the sole manifestation of ophthalmoplegic migraine. Walsh and O'Doherty7 presented specific criteria for the diagnosis of the syndrome: 2. Ophthalmoplegia including one or more nerves and possibly alternating sides with attacks. Extraocular muscle paralysis may occur with the first attack of headache or, rarely, precede it. However, the paralysis usually appears subsequent to an established migraine pattern. 3. Exclusion of other causes Hansen et al 8 found an annual incidence of 0.7 per million inhabitants for ophthalmoplegic migraine.? In a review of 5,000 migraine patients, Friedman et. al9 found 8 patients with ophthalmoplegic migraine, thus attesting to its rarity (0.16%). All 8 patients (5 male and 3 female) had periodic migraine headaches and unilateral ophthalmoplegia. Three patients had persistent ophthalmoplegia after years, and 1 had a definite family history of migraine. Six patients had arteriograms during the attacks; all results were normal. The details of this review are listed below: Number of attacks: 4 patients with 20+ attacks; 2 patients with 5 to 10 attacks; 2 patients with less than 5 attacks; and 1 patient with a single attack. Age at onset: 2, 2, 3, 3, 5, 8, 17, and 30 years. Clinical findings: Oculomotor paresis in all; pupillary involvement in 7. Pain: Always on the same side as ophthalmoplegia. Paresis: Occurred 3 to 5 days after onset of headache in 6 patients. Recovery: 1 to 4 weeks. Arteriogram: Normal in attack in 6 of 6. Therapy: Limited success. ? In ophthalmoplegic migraine the third nerve is most frequently involved. Walsh and Hoyt10 state that abducens palsy occurs 1:10 as frequently as third nerve palsy, with even rarer affliction of the fourth nerve. In most cases positive family history is not present. Thus, a typical clinical syndrome emerges: a child or young adult with periodic headache has ophthalmoplegia involving all functions of the third nerve, beginning at the height of an attack of cephalgia, which is primarily unilateral and in the orbital region; the paresis lasts for days to weeks following the cessation of headache; recovery is gradual and tends to be less complete after repeated attacks. The present case report is quite typical of those reported elsewhere: It also demonstrates that ophthalmoplegic migraine may selectively affect some? fibers of the oculomotor nerve.? In the differential diagnosis, consideration should be given to aneurysm, tumor, diabetes, and sphenoid sinus mucocele. The age at onset, negative glucose tolerance test, and radiologic studies will usually rule out the listed possibilities. Other clinical entities confused with ophthalmoplegic migraine have included myasthenia gravis and the Tolosa-Hunt syndrome. The former condition is ruled out if the pupil is involved (and actually should not be considered in the presence of pain) and with response to edrophonium chloride (Tensilon); the latter possibility should be considered if pain persists. On rare occasions only limited involvement of the third nerve occurs. ? Rarely, ophthalmoplegic migraine may occur without headache. Durkan et al14 described two children with isolated recurrent painless oculomotor palsy in whom neurodiagnostic investigations were all normal.? Opthalmoplegic migraine is a diagnosis of exclusion, and noninvasive imaging tests such as magnetic resonance imaging (MRI) or magnetic resonance angiography (MRA) should be performed in all cases to exclude the possibility of aneurysm6. ?Aneurysmal third nerve palsies are extremely rare in children under age 14 years15. ?However, in third nerve palsy involving pupillomotor function, serious consideration should be given to angiography. The usual cause will be a posterior communicating artery aneurysm, which is best excluded by conventional angiography. However, newer techniques such as MRA or spiral contrast-enhanced computed tomographic scanning may soon provide sufficient resolution to exclude aneurysm as a cause6. ? The pathophysiology of ophthalmoplegic migraine remains obscure. Theories include swelling of the posterior cerebral artery, pituitary swelling, vascular anomaly with compression of the third nerve, and unilateral brain swelling. None of these theories has been documented, and cerebral angiography is unrevealing. Walsh and O'Doherty7 suggested that a swollen intracavernous carotid artery compressed adjacent cranial nerves within the cavernous sinus. Such swelling would also narrow the vessel, which they attempted to document angiographically. However, subsequent negative arteriograms during attacks do not support this theory9. ?In Nigeria, ophthalmoplegic migraine has been associated with an abnormal hemoglobin16. The demonstration by magnetic resonance imaging (MRI) scanning of thickening and enhancement of the cisternal part of the oculomotor nerve in patients diagnosed as "ophthalmoplegic migraine" has prompted others to reconsider this uncommon disorder being a recurrent demyelinating neuropathy17. Carlow18 suggests that the pathophysiology may be a trigeminovascular migraine epiphenomenon that is dependent on the unique oculomotor nerve anatomy and porous blood-nerve barrier at the emergence of the oculomotor nerve from the brainstem and the sequelae of demyelination. Early high-dose corticosteroid treatment is recommended to rapidly resolve an acute episode and to potentially prevent permanent abnormal oculomotor nerve signs. Others speculate that the enhancing, thickened lesion identified on MRI may represent an inflammatory process similar to Tolosa-Hunt syndrome occurring in the interpeduncular segment of the oculomotor nerve3,19. Leone et al20 have speculated that tyramine eyedrop response suggested parasympathetic hypofunction on the affected side.Ideally, prophylactic therapy would prevent the occurrence of repeated episodes and prevent the development of permanent eye muscle palsies, but reports suggest that therapy has met with only limited success9. ?A trial with calcium channel blocking drugs such as verapamil or beta blocking drugs such as propranolol or even methysergide may be warranted if the attacks are frequent. In a case reported by Japanese observers21 the frequency and symptoms of migraine were remarkably reduced by topical administration of 0.25% timolol maleate twice daily to both eyes.? Others have found cyproheptadine hydrochloride quite useful in preventing recurrent attacks22. Based on a recent suggestion that prostaglandins' release (especially PGE1 and PGF2alpha) play a key role in the development of the migrainous attack. Rabey et al 23 found a therapeutic trial with flufenamic acid (a prostaglandin inhibitor of the fenamates group) to be quite successful.? Given the fact that this entity is probably similar to Bell's palsy one now may consider initial treatment with steroids and perhaps antiviral agents such as famcyclovir. ? References ?????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????????? 1. Vahlquist B: Migraine in children. Int Arch allergy Appl Immunol 1955;7:348 2. Bille B: A Study of the incidence and short term prognosis, and a clinical, psychological and encephalographic comparison between children with migraine and matched controls. Acta Pediatr Scan 1962;51:1 3: Wong V, Wong WC: Enhancement of oculomotor nerve: a diagnostic criterion for ophthalmoplegic migraine? Pediatr Neurol. 1997 Jul;17(1):70-3 4:Mark AS, Casselman J, Brown D, Sanchez J, Kolsky M, Larsen TC 3rd, Lavin P, Ferraraccio B: Ophthalmoplegic migraine: reversible enhancement and thickening of the cisternal segment of the oculomotornerve on contrast-enhanced MR images. 5: Troost BT, Tomsak RL: Ophthalmoplegic Migraine and Retinal Migraine, in Olesen J, Tfelt-Hansen P, Welch KMA (eds): The Headaches. New York, Raven Press Ltd. 1993:421-426. 6. Tomsak RL, Masaryk TJ, Bates JH: Magnetic resonance angiography (MRA) of isolated aneurysmal third nerve palsy. J Clin Neuro-ophthalmol 1991;11:16-18. 8. Hansen SL, Borelli-Moller L, Strange P, Nielsen BM, Olesen J ; Ophthalmoplegic migraine: diagnostic criteria, incidence of hospitalization and possible etiology. 10 Walsh FB, Hoyt WF: Clinical Neuro-Ophthalmology, Baltimore, Williams & Wilkins; 1969: 11. Hallet M, Cogan DG: Episodic unilateral mydriasis in otherwise normal patients. Arch Ophthalmol 1970;84:130 12. Edelson RN, Levy DE: Transient benign unilateral pupillary dilatation in young adults. Arch Neurol 1974;31:12 13. Woods D, O'Connor PS, Fleming R: Episodic unilateral mydriasis and migraine. Am J Ophthalmol 1984;98:229-234. 14. Durkan GP, Troost BT, Slamovits TL, et.al. Recurrent painless oculomotor palsy in children: a variant of ophthalmoplegic migraine. Headache 1981;21:58 15. Gabianelli EB, Klingele TG, Burde RM: Acute oculomotor nerve palsy in childhood. Is arteriography necessary? J Clin Neuro-ophthalmol 1989;9:33-36. 16. Osuntoken O, Osuntoken BO: Ophthalmoplegic migraine and hemoglobinopthy in Nigerians. Am J Ophthalmol 1972;74:451 17. Lance JW, Zagami AS; Ophthalmoplegic migraine: a recurrent demyelinating neuropathy? Cephalalgia. 2001 Mar;21(2):84-9 18. Carlow TJ: Oculomotor ophthalmoplegic migraine: is it really migraine???? J Neuroophthalmol. 2002 Sep;22(3):215-21 19. O'Hara MA, Anderson RT, Brown D. Magnetic resonance imaging in ophthalmoplegic migraine of children. J AAPOS. 2001 Oct;5(5):307-10 20. Leone M, Grazzi L, Moschiano F, Bussone G. Internal ophthalmoplegia associated with migraine attacks. Cephalalgia. 1994 Dec;14(6):461-2 21. Ishikawa H, Yoshihara M, Mizuki K, Kashima Y ; A pediatric case of ophthalmoplegic migraine with recurrent oculomotor nerve palsy ;Nippon Ganka Gakkai Zasshi. 2000 Mar;104(3):179-82. 22: Sugiyama N, Hamano S, Tanaka M, Mochizuki M, Nara T; MRI findings and effectiveness of cyproheptadine in two patients with ophthalmoplegic migraine.??? 2002 Nov;34(6):533-7 23: Rabey JM, Vardi Y, Van Dyck D, Streifler M: Ophthalmoplegic migraine: amelioration by Flufenamic acid, a prostaglandin inhibitor. Ann Neurol 1986;19:515-516. |
||


 ????????????????????????????????????????????????????????????
???????????????????????????????????????????????????????????? 